Caudal block
Dr Steve Roberts
Content
Indications
Specific contraindications
Anatomy
Technique
Volume of LA
Specific complications
Self-Assessment
Bibliography
Indications
A caudal block provides intraoperative and postoperative analgesia for infraumbilical and lower limb surgery.
In children older than 2 years of age cephalad spread is increasingly unreliable; in these circumstances alternative techniques e.g. truncal block or direct lumbar/thoracic epidural should be considered.
Specifically, it may be useful for the following operations:
- Circumcision
- Hypospadias
- Lower abdominal surgery e.g. ilioinguinal hernia repair
- Lower limb surgery e.g. club foot correction
Caudal catheters will be discussed in a separate section.
Specific contraindications
Spinal dysraphism (not cutaneous stigmata of spinal dysraphism, US allows screening of the spine).
Anatomy
- The caudal epidural space is the lowest section of the epidural space and is entered via the sacral hiatus.
- The non-fusion of the laminae of S5 and/or S4 creates the sacral hiatus.
- The sacral canal is a continuation of the lumbar spinal canal, which terminates at the sacral hiatus.
- The dural sac finishes at the L2 level (with a range of T10-L3) in term infants, and in preterm infants at L4.
- US does not pass through bone.
- With increasing age the spine becomes increasingly ossified, so diminishing the size of the echo windows (the view between the intervertebral spinous processes and laminae).
- The more cephalad the smaller the echo windows are compared to the ossified sections of the spine; particularly as the spinous processes become more angulated.
ECHO window : Ossification
| Caudal | 2:1 |
| Lumbar | 1:1 |
| Thoracic | 1:2 |
- In neonates and infants a midline sagittal probe position provides a good view; but with increasing age and lumbar/thoracic spine scanning a paramedian position increases the echo window size.
- The dural sac is hyperechoic (white) and its’ termination is readily identified. Within the dural sac the CSF is anechoic (black), the cauda equina is seen within as multiple hyperechoic lines.
- The thickest line within the cauda equina is the filum terminale, it should not be more than 2mm thick. Greater than 2 mm is an indication of spinal cord tethering.
- A tethered cord also has the following features: pulseless, the cord is positioned more posteriorly within the spinal canal.
Fig 1. Ultrasound Probe in Midline Transverse position over the coccyx.
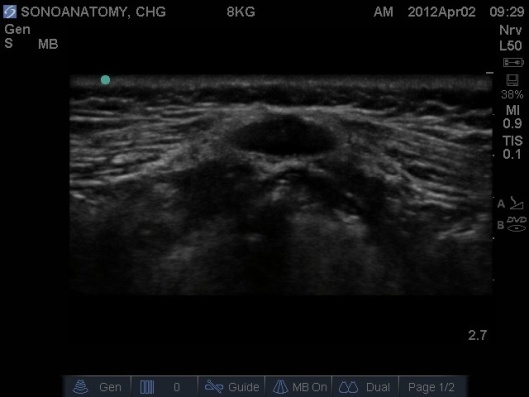
Fig 2. Ultrasound Probe in Midline Transverse position over the coccyx.
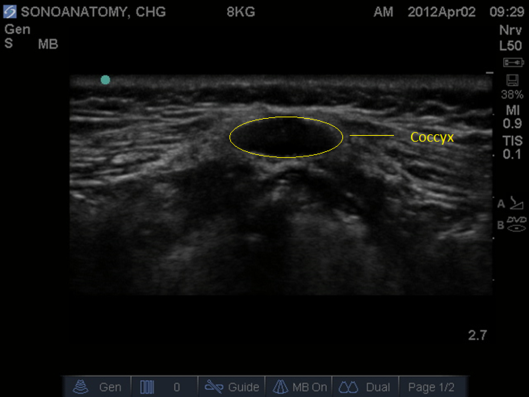
Fig 3. Ultrasound Probe in Midline Transverse position moved cephalad along sacrum.
C – sacral cornu, white asterisk sacrococcygeal membrane.

Fig 4. Ultrasound Probe in Midline Longitudinal position over sacrum.

Fig 5. Ultrasound Probe in Midline Longitudinal Plane over sacrum. D – dura, SCM – sacrococcygeal membrane
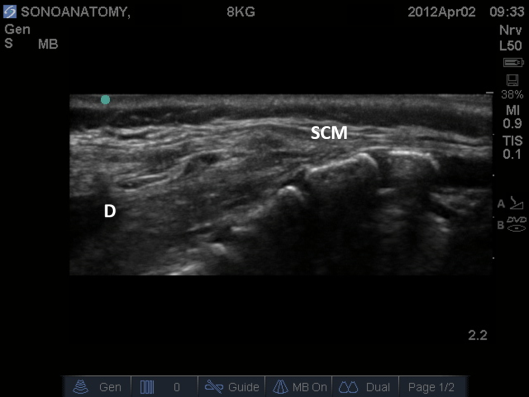
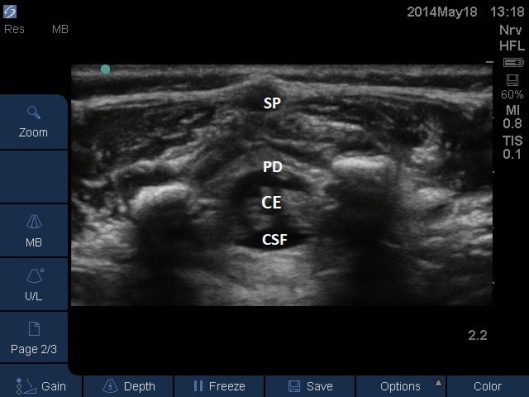
Fig 6. Ultrasound Probe in Midline Longitudinal position over the sacrum. CE = cauda equina. CSF = ceerbrospinal fluid (anechoic), PD = posterior dura (hyperechoic), SP = spinous process.

Fig 7. Ultrasound Probe in Midline Transverse position over the sacrum. CE = cauda equina. CSF = ceerbrospinal fluid (anechoic), PD = posterior dura (hyperechoic), SP = spinous process.
Technique
- This block is easily performed without US, but assessment of correct cannula placement has remained an issue despite various tests being introduced. The serious complications of intravascular and intrathecal injection remain a concern.
- Where the block is difficult (in the author’s opinion this is defined as being unable to place the cannula within 2 attempts) US can be used to guide the cannula/needle. An in plane needling technique is employed with the probe in the midline sagittal plane.
- Place the patient in the standard left lateral position with hips and knees flexed.
- The US machine should be positioned on the opposite side of the trolley to that where the operator is stood, i.e. in direct line of sight.
- Prior to performing the caudal a ‘Mapping’ or ‘Scout’ scan is performed to assess the position of the dural sac in relation to the sacrococcygeal membrane. The angle of needle/cannula insertion can be observed. See Figs 1-7.
- A large foot print linear probe (35mm) is ideal as it allows more intervertebral levels to be viewed, this is particularly useful when monitoring the spread of the LA or the migration of a caudal catheter.
- The probe should be placed in a transverse plane over the sacral hiatus first, then rotate the probe into a midline sagittal plane (the left of the screen should be cephalad).
- Perform the caudal as you normally would.
- The author’s preferred technique is to insert the cannula at the very apex of the sacral hiatus perpendicular to the skin. Once resistance is felt re-angle the needle to approx. 30 degrees and insert a further 5mm, then slide the cannula off the needle (it should slide off easily).
- Open the cannula to air and observe for blood or CSF.
- Then aspirate with a 2ml syringe.
- If the fluid is blood stained and not obviously in a vessel leave the cannula in position and wait to see what happens with the saline test bolus.
- Position the probe in the midline sagittal plane again, the cannula/needle may be visible. See Fig 8 below.
Fig 8. Ultrasound probe in Midline Longitudinal Plane, needle observed entering caudal space from right top hand corner of screen.

- Inject <0.1ml/kg of normal saline (this avoids wasting valuable LA, and is harmless if injected intravasculalry). See Fig 9 and 10 below. Where the posterior dura can be observed moving anteriorly as the epidural space is expanded.
Fig. 9 Patient in left lateral, cannula in situ with 2 ml syringe of saline attached. Note use of large footprint probe to give greater view of spine and observe for test injection.

Fig 10. Ultrasound probe in Midline Longitudinal position, saline test bolus seen as anechoic area displacing the posterior dura anteriorly.

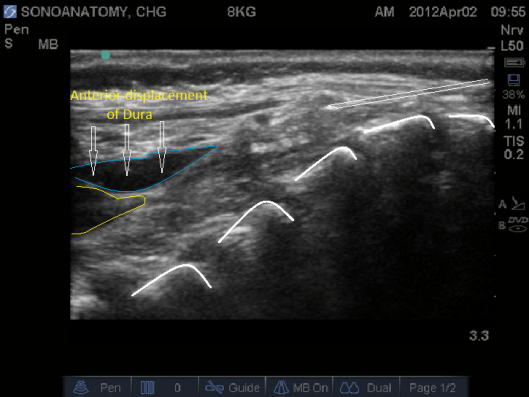
- Correct cannula position will see the test bolus of saline expand the epidural space, displacing the posterior dura anteriorly.
- If the saline test bolus is not seen then either the cannula/needle is in a vessel or the probe is not positioned correctly (check your probe position).
- After a positive saline test bolus attach your LA.
- The LA spread can be monitored to ensure it has spread high enough for the intended surgery. See Fig 11,12 and Video
- In neonates the probe can stay in the midline sagittal position, in older children it will be necessary to use the paramedian sagittal views (left and right) as the echo windows are greatest between the laminae. The probe moves synchronously cephalad as the LA spreads higher.
- Aspirate repeatedly during the block.
- Ensure the syringe is tightly attached to the cannula/needle as it is easy to be distracted by the US images and for the cannula to become displaced by a lack of attention.
Fig 11. Ultrasound Probe in Midline Longitudinal position over the lumbar spine. White * indicates local anaesthetic seen as anechoic area in posterior epidural space. CM = conus medullaris (anechoic with hyperechoic outline) with hyperechoic linear pattern of cauda equine attached.

Fig 12. Ultrasound Probe in Midline Transverse position over the lumbar spine. White * indicates local anaesthetic seen as anechoic area in posterior epidural space.

Volume of LA
- The volume injected must not be greater than the maximum possible dose. Spread of local anaesthetic within the epidural space should be monitored with US to ensure the appropriate level is reached for the intended operation.
- For neonates 0.125% levobupivacaine is effective and allows a greater volume to be injected should a mid thoracic level be desired (and an alternative technique e.g. direct thoracic epidural or caudal catheter is considered less appropriate).
Specific complications
- Intravascular injection.
- Spinal injection.
- Failure or inadequate block.
Top tips
- Use US to screen patients with cutaneous markers of spinal dysraphism.
- Use a saline test dose (safe if injected intravascularly and does not waste precious LA).
- If saline test dose not visible are you scanning in the wrong area or is the cannula intravascular?
- In neonates use 0.125% levobupivacaine as this is equally effective and minimises dosage.
Bibliography
http://www.sonographycme.com/cfm/lectures/lect001001.cfm
Park JH, Koo BN, Kim JY, Cho JE, Kim WO, Kil HK: Determination of the optimal angle for needle insertion during caudal block in children using ultrasound imaging. Anaesthesia 2006; 61: 946-9.
Roberts S A, Guruswamy V, Galvez I. Caudal injectate can be reliably imaged using portable ultrasound–a preliminary study. Paediatr Anaesth 2005; 15: 948-952.
Lundblad M, Lonnqvist PA, Eksborg S, Marhofer P. Segmental distribution of cuadal anesthesia (1.5 ml kg−1) in neonates, infants and toddlers as assessed by ultrasonography. Paediatr Anaesth 2011;21:121–7.
