Supraclavicular
Author: Dr. Nuria Masip
1. Indications
Supraclavicular block provides intraoperative and postoperative analgesia for all procedures on the upper extremity not involving the shoulder (1).
2. Specific contraindications
- Local infection
- Supraclavicular block should not be done bilaterally because of the potential respiratory problems originating from complications such as phrenic nerve block or pneumothorax (2).
3. Anatomy
The Brachial Plexus (3) is formed from the anterior primary rami of C5, C6, C7, C8 and T1. These nerve roots emerge from the intervertebral foramina between the anterior scalene and middle scalene muscles, being enclosed by a fascial sheath from these muscles.
The nerve roots unite to form trunks:
- C5 and C6 unite to form the superior trunk
- C7 forms the middle trunk
- C8 andT1 roots unite to form the lower trunk.
These trunks continue distally towards the axilla, sandwiched between the anterior scalene muscle (anteromedially) and the middle scalene muscle (posterolaterally), running parallel and supero-posterior to the subclavian artery, which is also enclosed by the fascial sheath.
As these trunks pass posterior to the clavicle, each trunk bifurcates into anterior and posterior divisions, which will reunite in the three cords of the brachial plexus:
- The anterior divisions of the upper and middle trunk unite to form the lateral cord
- The anterior division of the lower trunk forms the medial cord
- The posterior divisions of the three trunks unite to form the posterior cord.
These cords are named based on their relation to the axillary artery and divide into the nerves that supply the upper limb.
- Lateral cord – Lateral root of median nerve, Musculocutaneous nerve
- Medial cord – Medial root of median nerve, Ulnar nerve, Medial cutaneous nerves of arm and forearm
- Posterior Cord – Axillary and Radial nerves
4. Technique
- Position the patient in a semi-sitting position (this reduces the venous pressure in the neck) and turn patient’s head slightly away from the block site. In very small patients, shoulders should be elevated.
- Use a high frequency linear probe (> 10 MHz).
- A small footprint 25 mm linear probe.is desirable with smaller patients <15kg.
- The ultrasound machine is positioned on the far side of the patient, with the operator stood on the side to be blocked. The dominant hand manipulates the needle (which enters from lateral to medial).
- Using the non-dominant hand place the probe over the supraclavicular fossa, parallel to the clavicle, looking down into the chest. See Fig.1

Fig 1. Patient and probe position, note the head ring and a shoulder support, this allows better needle access.
- The probe should be angled/tilted till an optimal image is obtained where we can clearly identify these four structures: the subclavian artery, the first rib, the pleura and the brachial plexus.
- The first structure to locate is the round pulsating hypoechoic subclavian artery (A), lying on top of the hyperechoic first rib (R). Use Doppler to assess for vessels. See Fig. 2.

Fig. 2. Bidirectional Doppler used here to highlight the subclavian artery.
- The subclavian vein (V) is found more medially to the artery. The anterior scalene muscle inserts onto the first rib between these two vessels (A and V), but occasionally there are anatomical variations (4) where both vessels are together between the insertions of both the scalene muscles (anterior and middle ones).
- Quite often the dorsal scapular artery is seen coming off the subclavian artery and passing through the brachial plexus. See Fig. 9.
- A linear hyperechoic structure immediately deep and lateral to the A is the first rib with its bony shadow. However, in small children the cortical layer of ribs is thin enough that you can see both layers of the rib cortex and visualise lower down another bright line: the parietal and visceral pleura interface. See Fig. 3.
- Identify also another linear hyperechoic structure, which will be the pleura. Note the air artefact (the “comet tail” sign) and the pleura sliding movement during respiration.
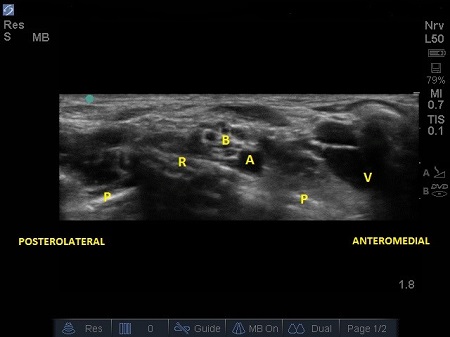
Fig. 3. Sonoanatomy of infant supraclavicular region. A – Subclavian artery. B – brachial plexus, P – pleura, R – first rib, V – subclavian vein
- A mirror or reverberation artefact of the Subclavian Artery often occurs, mimicking a second Subclavian Artery beneath the rib. See Fig.
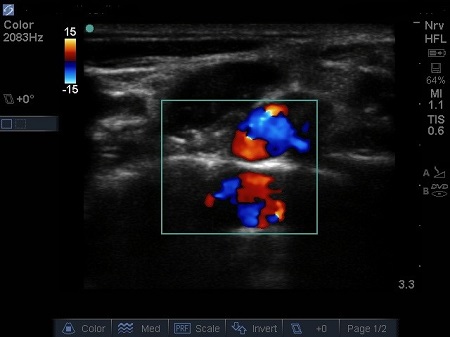
Fig.4. Mirror artefact of subclavian artery
- Lateral and above the artery sit a bundle of round hypoechoic circles (“bunch of grapes” or “cluster of bubbles”) – the brachial plexus, at this level, the plexus will be configured as trunks and/or divisions.
- It may be possible to identify the hypoechoic nodules surrounded by a hyper-reflective fascial sheath.
- When the plexus is difficult to identify, it can be useful to follow it proximally in the neck (in the interscalene space).
In plane technique:
- VIDEO LINK
- Introduce the needle from the lateral side of the probe advancing medially. See Fig. 5.

Fig. 5. Needle introduced from posterolateral to anteromedial, bevel up.
- Position the needle within the sheath, often a “pop” is felt as the needle passes through the brachial plexus sheath.
- Local anaesthetic (LA) should spread around the hypoechoic circles causing hydro dissection of the planes. (5) See 6. & 7.

Fig. 6. Initial injection of LA, note proximity to subclavian artery. Excellent needle control is required to safely perform this technique.
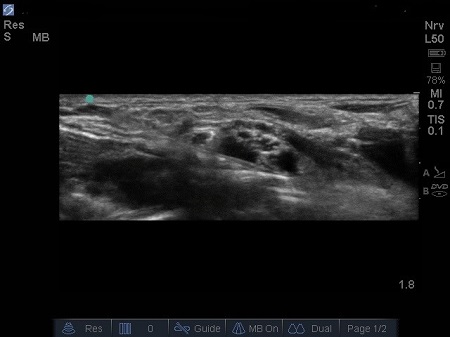
Fig. 7. Increasing spread of LAj
- It may sometimes be necessary to reposition the needle to ensure an adequate distribution of the LA (the entire plexus is surrounded by LA). See Fig. 8.
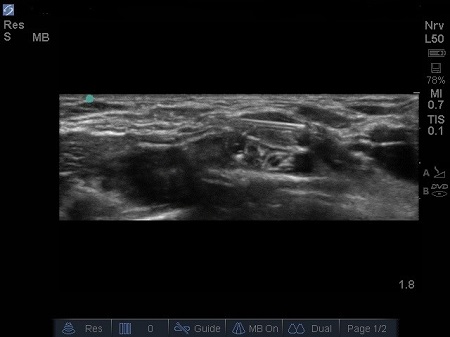
Fig. 8. Needle withdrawn and re –directed over the superior aspect of the brachial plexus, LA deposited to surround brachial plexus.
- Never inject against high resistance, this may be a sign of an intrafascicular injection.
- Although, there will be slightly more resistance when initially injecting within the sheath than normally felt outside the sheath, but the resistance will ease quickly. The LA will then be distributed cephalad and caudally within the sheath.
- If anaesthesia is intended for the distal upper limb, aim to spread LA in the corner bordered by the subclavian artery medially, the first rib inferiorly, and the divisions of the brachial plexus superior laterally (“the corner pocket”, and the ulnar nerve in this position would be “the 8-ball”) (6) (7).
- The safety of positioning the needle tip within the brachial fascia sheath and spreading LA among the neural clusters is controversial:
- In a 2009 observational study, Bigeleisen et al. (8) opined that positioning the needle tip inside a cluster equated to intraneural placement (and intraneural LA injection).
- In contrast, in a further publication, Franco (9) argued “penetrating the prevertebral fascia during an interscalene or supraclavicular block, for example, does not constitute intraneural injection as has been erroneously postulated, unless the individual epineurium of the individual nerve structures (roots, trunks, or divisions) is penetrated.”
- Regardless of whether LA is deposited inside the neural cluster amounts to true intraneural injection or not (10) (11), it seems to be safe and therefore is the approach described here.
5. Volume of LA
Generally 0.3-0.5ml/kg is used, but doses as low as 0.1–0.2 ml/kg of 0.25% Levobupivacaine can be used successfully.
6. Potential complications
- Pneumothorax (12, 13) – careful when positioning needle in “the corner pocket”.
- Phrenic nerve block (~50%, due to proximal spread of the LA within the sheath).
- Horner’s syndrome (~1%)(14) (due to proximal spread of the LA within the sheath and blockage of sympathetic afferents).
- Unintended vascular punctures (~0.4%)(14)
- Intravascular injection with LA toxicity.
- Neurological injury (15) (rare) – most are temporary rather than permanent.
7. Top tips
Always use US in children when performing this block.
Before performing the block, four structures must have been identified: the subclavian artery, the two linear hyperechoic structures (first rib and pleura) and the brachial plexus, all these structures should be kept in view.
Hypoechoic vessels may be seen among the brachial plexus nerves (also round hypoechoic structures). Because they have similar appearance, it is important to differentiate them (colour Doppler MUST be used) (16). See Fig. 9.
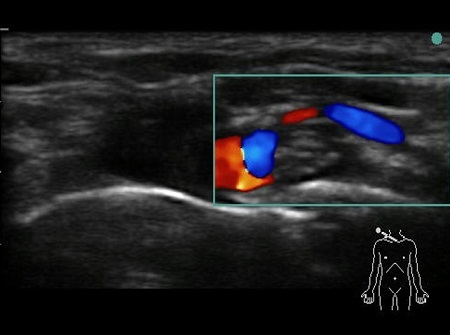
Fig. 9. Doppler highlighting subclavian artery with dorsal scapular artery passing posteriorly through brachial plexus.
When the plexus is difficult to identify, it can be useful to scan higher in the neck finding the nerve roots sandwiched by the scalene muscles and follow them down.
If the block is performed for hand surgery, it is important to spread the local anaesthetic near the inferior trunk, this is situated in the most dangerous area (risk of pneumothorax) where the artery meets then rib/pleura (“the corner pocket”).
When placing catheters an in plane technique can be used, by inserting the needle from a more posterior position the catheter can be self-tunnelled. When using a needle with a Huber tip it may be useful to aim the bevel caudad and lateral with a view to threading the catheter in the direction the brachial plexus is travelling. See Fig. 10.

Fig. 10. Longitudinal view of peripheral nerve catheter positioned beneath brachial plexus.
8. Bibliography
- Marhofer P, Lonnqvist PA. The use of ultrasound-guided regional anaesthetic techniques in neonates and young infants. Acta Anaesthesiol Scand. 2014;58:1049-1060.
- Gelpi B, Telang PR, Samuelson CG, Hamilton CS, Billiodeaux S. Bilateral ultrasound-guided supraclavicular block in a patient with severe electrocution injuries of the upper extremities. J La State Med Soc. 2014;166:60-62.
- Standring S. (ed.) 2008. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 40th Ed. Churchill Livingstone, Philadelphia. p 1–1576.
- Muhly WT, Orebaugh SL. Sonoanatomy of the vasculature at the supraclavicular and interscalene regions relevant for brachial plexus block. Acta Anaesthesiol Scand. 2011;55:1247-1253.
- Techasuk W, Gonzalez AP, Bernucci F, Cupido T, Finlayson RJ, Tran DQ. A randomized comparison between double-injection and targeted intracluster-injection ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2014;118:1363-1369.
- Soares LG, Brull R, Lai J, Chan VW. Eight ball, corner pocket: the optimal needle position for ultrasound-guided supraclavicular block.[letter]. Reg Anesth Pain Med 2007;32(1):94-95.
- De Jose Maria B, Banus E, Navarro Egea M, Serrano S, Perello M, Mabrok M. Ultrasound-guided supraclavicular vs infraclavicular brachial plexus blocks in children. Paediatr Anaesth. 2008;18:838-844.
- Bigeleisen PE, Moayeri N, Groen GJ. Extraneural versus intraneural stimulation thresholds during ultrasound-guided supraclavicular block. Anesthesiology. 2009;110:1235-1243.
- Franco CD. Connective tissues associated with peripheral nerves. Reg Anesth Pain Med. 2012;37:363-365.
- Morfey D, Brull R. Ultrasound-guided supraclavicular block: What is intraneural? Anesthesiology. 2010;112:250-1; author reply 251.
- Jeng CL, Rosenblatt MA. Intraneural injections and regional anesthesia: the known and the unknown. Minerva Anestesiol. 2011;77:54-58.
- Abell DJ, Barrington MJ. Pneumothorax after ultrasound-guided supraclavicular block: presenting features, risk, and related training. Reg Anesth Pain Med. 2014;39:164-167.
- Kakazu C, Tokhner V, Li J, Ou R, Simmons E. In the new era of ultrasound guidance: is pneumothorax from supraclavicular block a rare complication of the past?[letter]. Br J Anaesth 2014;113(1):190-191.
- Hanumanthaiah D, Vaidiyanathan S, Garstka M, Szucs S, Iohom G. Ultrasound guided supraclavicular block. Med Ultrason. 2013;15:224-229.
- Liu SS, YaDeau JT, Shaw PM, Wilfred S, Shetty T, Gordon M. Incidence of unintentional intraneural injection and postoperative neurological complications with ultrasound-guided interscalene and supraclavicular nerve blocks. Anaesthesia. 2011;66:168-174.
- Hahn C, Nagdev A. Color Doppler Ultrasound-guided Supraclavicular Brachial Plexus Block to Prevent Vascular Injection. West J Emerg Med. 2014;15:703-705.
