Transversus Abdominus Plane Block
Dr Richard Craig
Content
- Indications
Specific contraindications
Anatomy
Technique
Volume of LA
Specific complications
Self-Assessment
Bibliography
Indications
The Transversus Abdominis Plane (TAP) block provides intraoperative and postoperative analgesia for upper and lower abdominal incisions, where an epidural is contraindicated or considered too invasive for the minor nature of the surgery. TAP block has been described in paediatric patients for the following operations:
- Colorectal surgery e.g. colostomy formation
- Iliac Crest bone harvest site
- Inguinal hernia repair
- Laparoscopic and open Appendicectomy
- Laparoscopic cholecystectomy
- Laparoscopic nephrectomy
- Renal transplant recipients
Catheter techniques have also been described in the paediatric population.
Specific contraindications
Local infection at the proposed needle insertion point
Anatomy
- The skin of the anterior abdominal wall is supplied by the ventral rami of the inferior six thoracic nerves. These are the continuation of the T7 to T11 intercostal nerves and the subcostal nerve (T12).
- The ventral ramus divides into a lateral cutaneous nerve and an anterior cutaneous nerve. These innervate the skin of the anterior abdominal wall.
- The ventral rami of T 7 to T12 run in the plane between the transversus abdominis muscle and the internal oblique muscle – the Transversus Abdominis Plane.
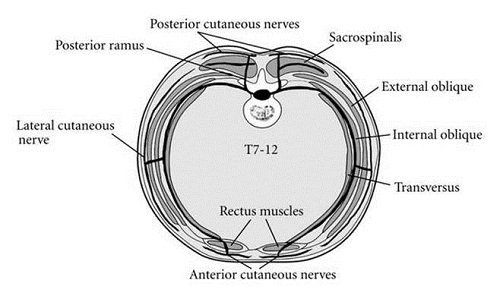
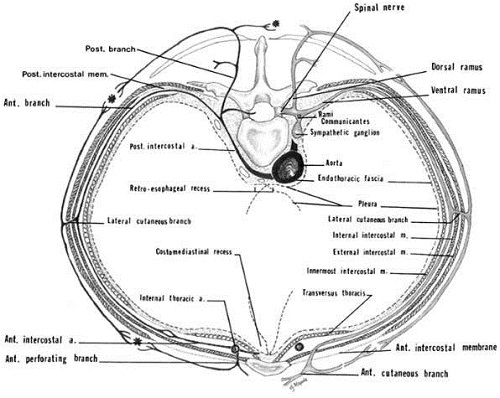
- The transversus abdominis muscle is the innermost of the flat muscles of the abdomen. It arises from the lateral third of the inguinal ligament, the anterior three-quarters of the iliac crest, the inner surfaces of the costal cartilages of the lower six ribs, and from the lumbodorsal fascia. Its insertion is the xiphoid process, the pubic crest and pectineal line (forms the conjoint tendon along with the internal oblique muscle aponeurosis) , and the linea alba (above the arcuate line it fuses with the posterior layer of the internal oblique aponeurosis to form the posterior wall of the rectus sheath, below the arcuate line the aponeurosis of transversus abdominis lies anterior to the rectus abdominis muscle.
- The transversalis fascia and the peritoneum are deep to the transversus abdominis muscle.
- The quadratus lumborum muscle arises from the iliolumbar ligament and the adjacent portion of the iliac crest, and is inserted into the lower border of the 12th rib, and by four small tendons into the apices of the transverse processes of the L1 to L5 lumbar vertebrae.
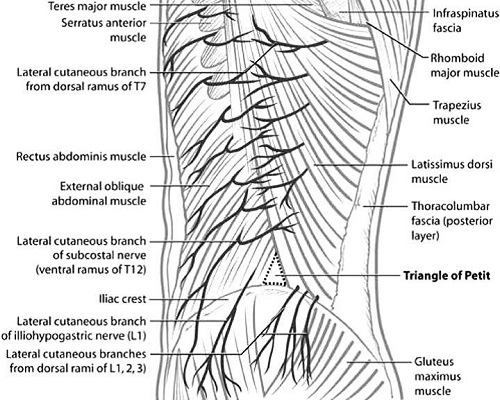
- The lumbar triangle of Petit is used to determine the needle insertion point in the landmark-based technique of performing a TAP block. The posterior border of the triangle is the latissimus dorsi muscle, the anterior border is the external oblique muscle, and the base is the iliac crest (Fig 3)
Technique
The following techniques have been described:
- Ultrasound-guided mid-axillary approach
- Ultrasound-guided anterior subcostal approach
Ultrasound-guided mid-axillary approach
- Position the patient supine.
- Select a linear probe
- The ultrasound machine is positioned on the far side of the patient, with the operator stood on the side to be blocked. For bilateral blocks less experienced operators will find the far side block harder to maintain needle visualisation.

- Place the ultrasound probe in a transverse plane between the iliac crest and the costal margin.

- Left-right probe orientation is easier if you start scanning over the linea alba in the midline and then move the probe laterally until it is between the iliac crest and the costal margin.
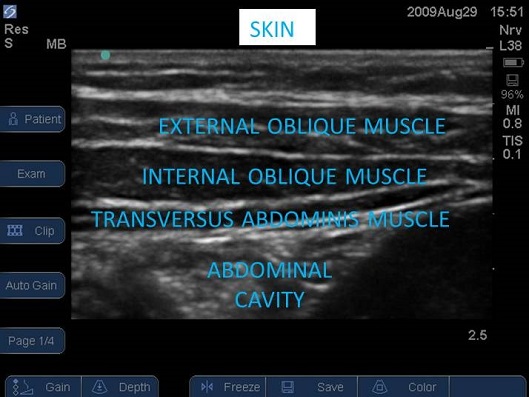
- Identify the peritoneum and then the lateral abdominal muscles from deep to superficial (transversus abdominis, internal oblique, and external oblique).
- In obese children fascial planes can appear within the subcutaneous adipose tissue, this can lead to confusion and misidentification of the muscle layers if the layers are identified from superficial to deep.
- The target is the fascial plane between the transversus abdominis and the internal oblique muscles.
- Use an in-plane needling technique . Choose a needle insertion point such that the needle is as perpendicular to the ultrasound beam as possible; this will result in the best possible image of the needle.
- Advance the needle in an antero-posterior direction.
- Aim to puncture the fascia on the deep aspect of the internal oblique muscle to have the needle tip on the transversus abdominis side of the fascial layer (a slight give or pop is often felt).

Figure 5 Ultrasound image of lateral abdominal wall of infant, needle inserted from anterior to posterior using an in plane needling technique. A 10MHz linear probe is positioned in the transverse plane midway between the iliac crest and costal margin.
- In neonates you should see a neat lens-shaped deposit of local anaesthetic forming between the transversus abdominis muscle and the fascia separating the internal oblique muscle and transversus abdominis (Fig 6). In older children strands can be seen stretching between the two muscles.
- Aim to deposit the injectate at the posterior part of the TAP; at or posterior to the mid-axillary line. There is potential to miss the L1 nerve branches should the injection be made too posterior as the nerve may not have passed into the TAP yet.

Figure 6 Ultrasound image of lateral abdominal wall of infant, needle inserted from anterior to posterior using an in plane needling technique. Note the spread of local anaesthetic between the inner most muscles. In small children it is common for the local anaesthetic to back track along the needle path as is seen here by the ‘fluffing’ of the interior oblique muscle.

- If you see local anaesthetic spreading within the internal oblique muscle superficial to the fascia between internal oblique and transversus abdominis, reposition the needle tip deep to the fascia.
- It can prove difficult to enter the TAP, if so; place the needle in the transversus abdominis muscle. As you withdraw the needle have an assistant inject, as the needle tip passes into the TAP space
Ultrasound guided anterior subcostal approach
- The patient is placed supine.
- The ultrasound probe is placed over the subcostal area in an oblique transverse plane, parallel to the subcostal margin. lateral to the rectus sheath.
- Identify the medial border of the external oblique, internal oblique and transversus abdominis muscles. Identify the TAP. Insert the block needle at the lateral edge of rectus abdominis. Advance the needle in-plane away from the midline and parallel to the costal margin. Hydro-dissect the plane.

Volume of LA
0.3-0.5ml/kg/side of 0.25% levobupivacaine.
Top Tip
Always use an in plane needling technique
Always identify the abdominal muscle from deep to superficial.
In larger patients (where a steeper angle of needle trajectory is required) needle enhancing software may improve the view.
If you are finding difficulty entering the TAP plane carefully enter the transversus abdmonis muscle with your needle. On withdrawing the needle have your assistant inject, as the bevel withdraws into the plane you will see a splitting of the muscle layers.
Specific complications
- Peritoneal perforation
- Organ perforation (in neonates the liver and spleen are particularly prominent)
Self-Assessment
- Unilateral TAP block is indicated for
a) Laparotomy
b) Cholecystectomy
c) Laparoscopic appendicectomy
d) Pyloromyotomy
e) Inguinal Herniorrhaphy - Label the image below
A anterior
B posterior
C Transversus Abdominis muscle
D Internal Oblique muscle
E External Oblique muscle
F Peritoneum

Bibliography
- Carney J, Finnerty O, Rau J, Curley G, et al. Ipsilateral transversus abdominis plane block provides effective analgesia after appendicectomy in children: a randomised controlled trial. Anesthesia & Analgesia. 2010. Vol. 111, 4, pp. 998-1003.
- Carney J, Finnerty O, Rauf J, et al. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011. Vol. 66, pp. 1023-1030.
