Thoracic Paravertebral Block
Dr Naveen Raj
Content
- Introduction
- Indications
- Specific contraindications
- Anatomy
- Technique
- Volume of LA
- Specific complication
- Bibliography
Introduction
Paravertebral block is a technique where local anaesthetic is injected into the space adjacent to the vertebrae to block the spinal nerves as they emerge from the intervertebral foramen. Here the spinal nerves are devoid of covering fascia making them sensitive to the action of local anaesthetics. The block is of high quality and sufficient to provide analgesia for major surgery at various sites. A single site injection can provide blocks of 4-6 dermatomes. It can be performed at the Cervical, Thoracic or Lumbar level; however only the Thoracic Paravertebral block will be discussed here.
Thoracic paravertebral block confers several advantages over epidural block:
- Comparable pain relief with reduced side effects.
- Better pulmonary function and fewer pulmonary complications
- Contraindications to thoracic epidural block do not preclude thoracic paravertebral block e.g. systemic sepsis, deranged coagulation
Indications
Both single shot unilateral or bilateral Paravertebral blocks and continuous infusions via placement of catheter into the site of block can be used to provide perioperative analgesia for various surgical procedures of the chest wall, thorax and abdomen (* indicates bilateral block).
- Thoracotomy
- Sternotomy * including cardiac and chest wall correction surgery
- Breast surgery
- Renal and Ureteric surgery
- Cholecystectomy
- Orchidopexy
- Fundoplication
- Appendicectomy
- Hernia repair
- Laparascopic procedures
- Major abdominal surgery
It also can be used in nonsurgical acute and chronic pain management:
- Fractured ribs
- Lung contusions
- Benign and malignant neuralgia
- Complex regional pain syndromes
Specific Contraindications
- Tumour in the paravertebral space
- Empyema
- Infection at site of block
- Caution in those with previous thoracotomy and chest deformities including kyphoscoliois
Anatomy
The Thoracic paravertebral space is a wedge shaped space adjacent to the Thoracic vertebral column. The boundaries of the space are:
- Medial – the vertebral body and intervertebral foramen.
- Antero-lateral – Pleura.
- Posterior – Costo-transverse ligament and the internal intercostal membrane laterally. These two structures are continuous with one another.
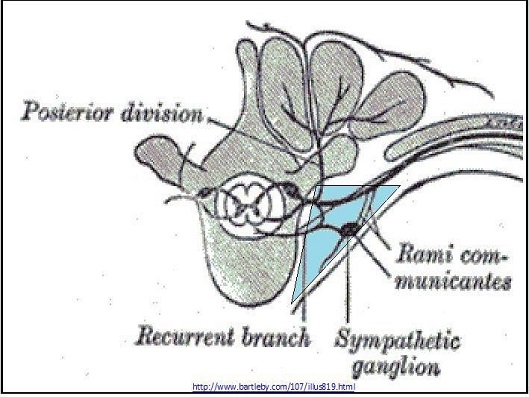
Fig 1. Boundaries of the paravertebral space
Contents of the space include:
- Adipose tissue
- Anterior ramus of Spinal (Intercostal) nerves
- Posterior ramus of Spinal (Intercostal) nerves
- Sympathetic chain
- Rami communicantes
Thoracic paravertebral space communicates with:
- Medially – Epidural space
- Laterally – Intercostal space
- Superiorly – Cervical paravertebral space
- Inferiorly –limited spread due to the origins of the Psoas Major muscle
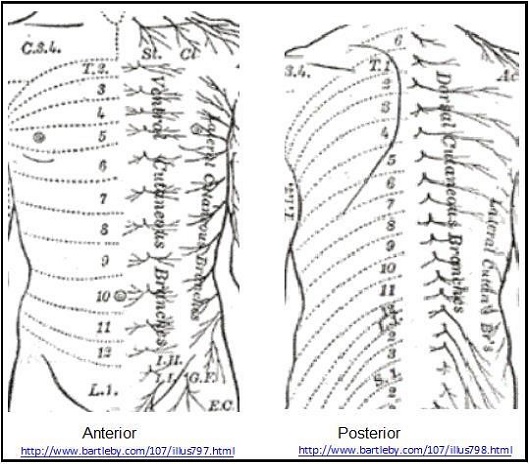
Eleven Intercostal nerves (T1-T11) and one Subcostal Nerve (T12) arise from spinal cord and exit the intervertebral foramen on both sides of the vertebral column to divide immediately into an anterior and posterior division.
- The posterior division – divides into medial and lateral branches and supplies the muscles and skin of the posterior part of the chest.
- The anterior divisions initially lie between the pleura and the posterior intercostal membrane and then continue between the innermost and inner intercostal muscles to terminate as the anterior cutaneous branch of the thorax. A lateral branch is given off midway between the vertebral body and the sternum approximately at the mid axillary line which in turn divides into anterior and posterior branches.
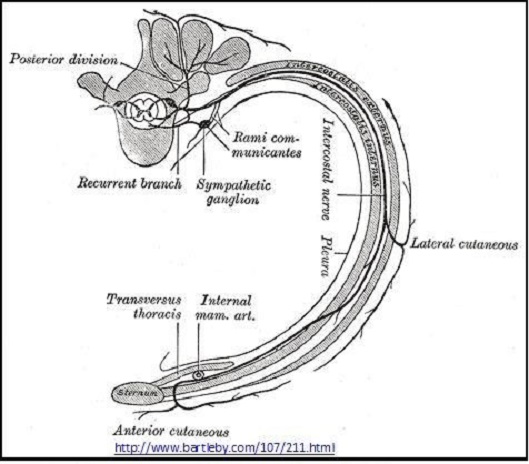
Fig 2. Course of the thoracic intercostal nerves
- The anterior divisions of T2 -6 are limited to the thorax and are called thoracic intercostals nerves.
- The anterior divisons of T7-T11 in addition continues into the abdomen to run between the Internal Oblique and Transverse Abdominis to supply skin and muscles of the anterior abdomen and hence are called thoracoabdominal intercostals nerves. They pierce the rectus sheath to terminate as the anterior cutaneous branches of the abdomen
- The anterior division of T12 runs along the lower border of the 12th rib and then into the abdomen similar to the lower intercostals nerves. The lateral branch does not divide into anterior and posterior division. It pierces the external oblique muscles and descends over the iliac crest to supply the skin over the front part of the gluteal region as far as the level of greater trochanter
Technique
- In our current practice the anaesthetised child is placed in the lateral position with the side to be blocked uppermost (fig 4A&B)). The block can also be done in the prone position and in those who are awake it is best done sitting up, leaning forward.
- Position the ultrasound machine appropriately, generally on the opposite side of the patient to the operator.

Fig 4A
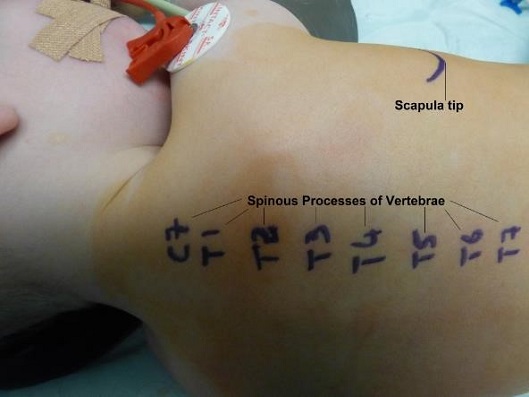
Fig. 4B
- Level of the block:
o T4 for Sternotomy
o T6 for Thoracotomy
o T10 for Abdominal procedures - Equipment: Standard block needle, 40-50mm length for small children and smaller, longer needles will be required for older children depending on needling technique used.
- If inserting a catheter then appropriate kit needs to be selected.
- Sterility: As there is epidural spread of the injectate all measures to maintain sterility should be taken. For single shot blocks we use a sterile non touch technique with gloves, drapes and US cover and sterile gel. When inserting catheters then full aseptic precautions are taken.
- Identify and mark the spinous process at the appropriate level where the block is to be done.
- There are 2 main approaches –
o A) Probe in transverse plane Fig 5
o B) Probe in sagittal plane Fig 6

Fig. 5

Fig. 6
A) Probe Transverse – Needle In-Plane Approach
- Select an appropriate sized US probe. For neonates and infants a 25mm linear probe, for older children a larger probe of approx. 35mm. is chosen.
- Place the probe in transverse plane over the midline at the chosen vertebral level
- Probe orientation preferred by the author – orientation mark is on medial side.
- Identify the spinous process (SP) of the thoracic vertebrae
- Move the probe laterally in this plane and view the lamina and lateral to this the hyperechoic transverse process (TP) with acoustic shadow beneath (Fig 7,8)

Fig 7. Transverse Plane Mid-Thoracic level. PVS – paravertebral space, SP – spinous process, TP – start of transverse process.
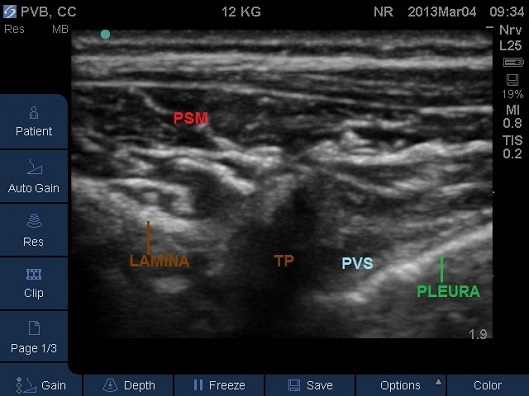
Fig 8. Transverse Plane Mid-Thoracic level. PSM – paraspinal muscles, PVS – paravertebral space, SP – spinous process, TP –transverse process.
- Identify the rib and intercostal muscles lateral to the transverse process (Fig 9).
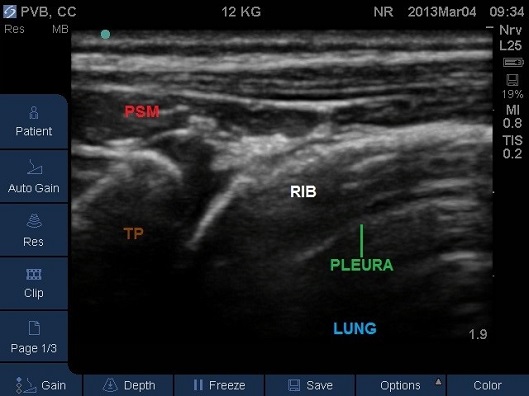
Fig 9. Transverse Plane Mid-Thoracic level. PSM – paraspinal muscles, TP – tip of transverse process
- Identify the pleura beneath (Fig 10). For the best view and a successful block you should ensure the pleura is visible as a bright white solid line with characteristic appearance of intercostal muscles above.
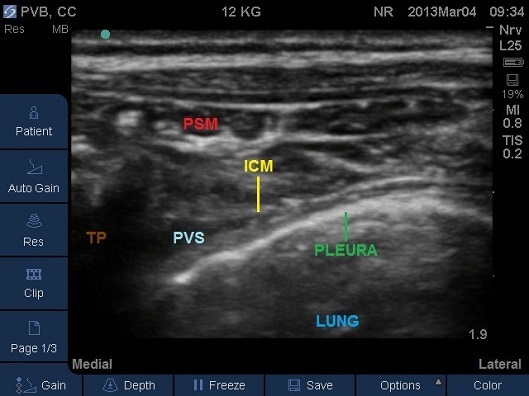
Fig 10. Transverse Plane Mid-Thoracic level. ICM – internal intercostal membrane, PSM – paraspinal muscles, PVS – paravertebral space, TP – tip of transverse process. Note the internal intercostal membrane is continuous with the costotransverse membrane.
- The transverse process with its acoustic shadow should be close to one end of the screen and opposite to the side of needle insertion.
- The needle should be inserted in-plane from the lateral to medial direction aiming for the junction of the pleura and the acoustic shadow underneath the transverse process (Fig 11).

Fig 11. Probe –needle position.
- The needle should pass through the intercostals muscle (Fig 12) and the needle tip should end in a hypoechoic triangular space formed by the acoustic shadow underneath the transverse process medically, pleural antero-laterally and the lower border of the intercostals muscles posteriorly. A subjective subtle “give” may be felt as the lateral costo-transverse ligament or internal costal membrane is pierced prior to entering the space.
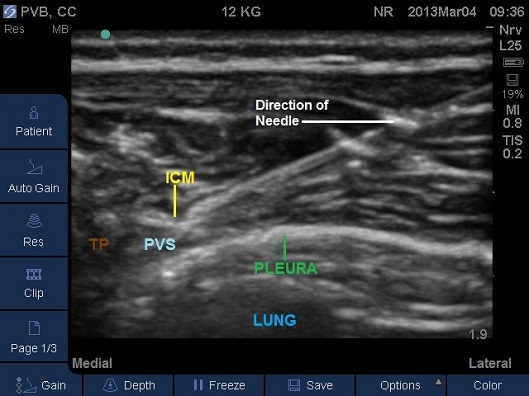
Fig 12. Transverse Plane Mid-Thoracic level showing in plane technique needle travelling lateral to medial. ICM – internal intercostal membrane, PSM – paraspinal muscles, PVS – paravertebral space, TP – tip of transverse process.
- Correct placement of the needle in the thoracic Paravertebral space should be confirmed by the anterior displacement of pleural upon injection of a small bolus of saline or local anaesthetic (Fig 13-16).
- Once confirmed the required volume of local anaesthetic should be injected.
- Watch the VIDEO of the paravertebral block in a 2kg neonate by clicking on the clipframe below
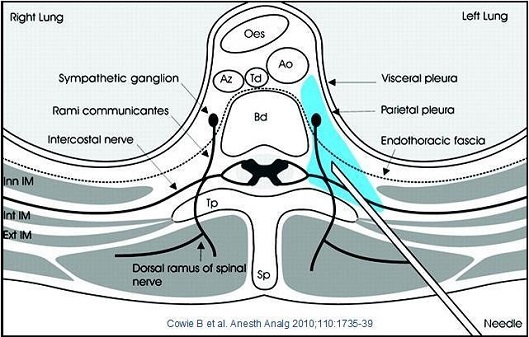
Fig 13.

Fig 14. Paravertebral space entered by needle, pleura displaced anteriorly by local anaesthetic.
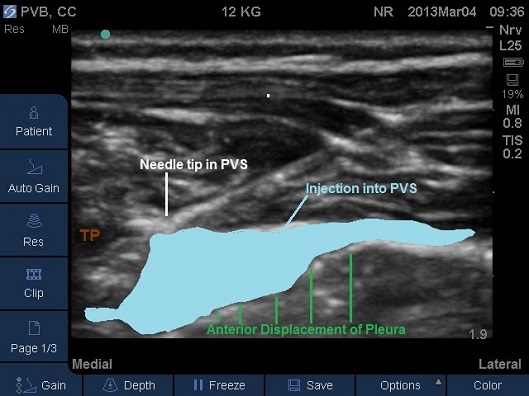
Fig 15. Paravertebral space entered by needle, pleura displaced anteriorly by local anaesthetic. TP –transverse process. Local anaesthetic spread marked in light blue

Fig 16. Paravertebral space filled by local anaesthetic. TP –transverse process.
- In cases where an appropriate size US probe is unavailable (35mm probe and infant combination) or in those situations where the rib or scapula comes in the way of completing the transverse intercostal in-plane approach as described above; then a Transverse Probe – Needle Out of plane approach can be implemented
- The needle is inserted at mid point of the probe and is directed in a perpendicular manner to the tissue planes to enter the paravertebral space. The needle is only visible as a white dot and tissue plane movement or injection of small volume of saline assists in ascertaining the position of the needle tip.
B) Probe Sagittal – Out of Plane Needle Approach
- Place an appropriate size US probe in sagittal plane over the midline. The spinous processes will be observed. Slide the probe laterally so that it is positioned parallel to the vertebral column.
- The level of the intended block should be in the middle of the probe.
- Move the probe laterally in the same plane to visualise the acoustic window between the transverse processes (Fig 17). The Paravertebral space is usually not clearly visible in this plane. Occasionally the costo-transverse ligaments can be identified. The pleura with lung beneath is clearly visible more anteriorly.
- Kamarkar et al have demonstrated that the ligaments and pleura are visualised better if the probe is tilted slightly lateral.

Fig 17. Probe – needle orientation for out of plane technique.
- Probe orientation preferred by the author – orientation mark is directed cranially.
- Identify the hyperechoic round transverse process with its anechoic shadow beneath (Fig 18).
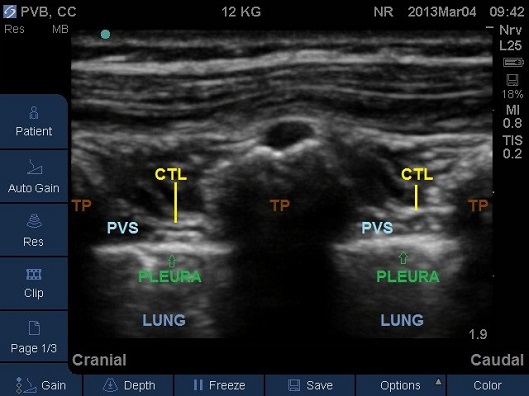
Fig 18. Parasagittal plane at mid-thoracic level. CTL – costotransverse ligament, PVS – paravertebral space, TP – transverse process.
- The needle should be introduced near the middle of the probe at the level of the lower transverse process. The needle should be aimed for the junction of shadow between the caudal part of the upper transverse process and the pleura.
- The needle will only be visible as a white dot; tissue plane movement or injection of a small volume of saline assists in ascertaining the position of the needle tip (Fig 19-20). Needle position is confirmed by the anterior displacement of pleura and widening of the Paravertebral space on injection.
Fig 19A and 19B. Parasagittal plane at mid-thoracic level showing initial injection of saline to assess needle tip position, note the anterior displacement of the pleura. TP – transverse process.

Fig 19A
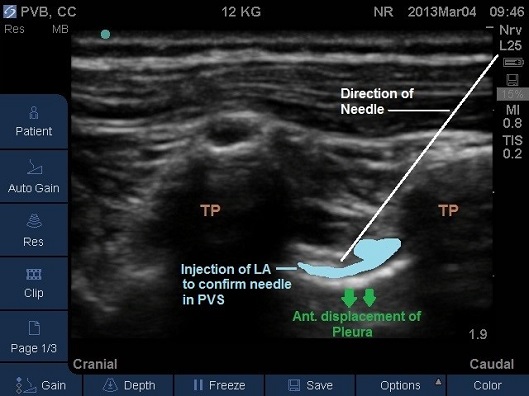
Fig 19B
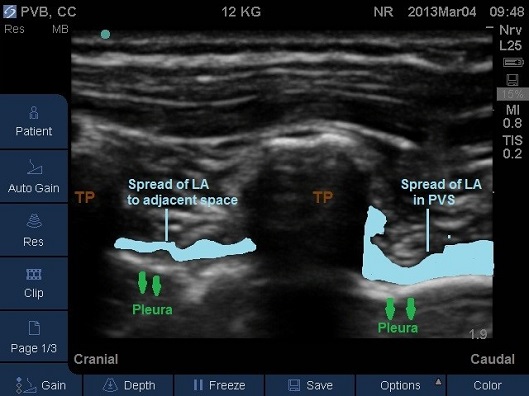
Fig 20A and 20B. Parasagittal plane at mid-thoracic level showing spread of local anaesthetic to adjacent paravertebral levels. TP – transverse process.

Fig 20A
- After careful aspiration local anaesthetic is injected.
- Spread can be assessed with ultrasound, in neonates spread into the epidural space may be observed.
- A catheter can then be inserted into the space so that the tip lies 2-3 cm beyond the tip of the needle. Catheter insertion is not easy and will require some needle manipulation.
- An In-plane approach is possible in bigger children and adults; the needle being introduced in plane from a caudal to cranial direction.
Local Anaesthetic and dosage
- Depends on availability and preference of the operator.
- L-Bupivacaine & Ropivacaine are commonly used.
- In our current practice we use 0.25% L-Bupivacaine, 0.3-0.5 ml-1 kg per side
- Adjunct drugs:
Clonidine or Fentanyl 1 to 2 micrograms-1 ml may be useful. With the spread of the local anaesthetic into the epidural space these adjuncts are useful in improving the quality and duration of the block. Clonidine can be associated with hypotension and bradycardia.
Side effects/complications
- Sympathetic blockade leading to hypotension and fall in heart rate.
- Epidural spread of local anaesthetic.
- Pneumothorax.
- Bleeding.
- Epidural/Intrathecal spread.
- Hypotension.
- Infection.
- Nerve injury.
Bibliography
- Manoj Kamarkar. Thoracic Paravertebral block. Anesthesiology 2001; 95:771-80
- Manoj Kamarkar. Ultrasound guided Thoracic Paravertebral block. Techniques in regional anesthesia and pain management 2009; 13: 142-9
- JE Chelly. Paravertebral blocks. Anesthesiology Clinics 2012; 30: 75-90
- J Richardson, PA Lonnqvist and Z Naja. Bilateral Thoracic Paravertebral Block: potential and practice. British Journal of Anaesthesia 2011; 106: 164-71
- Prema Thavaneswaran, Glenda Rudkin, Rodney Cooter, et al. Paravertebral block for anesthesia: a systematic review. Anesthesia and Analgesia 2010: 110: 1740-4
- A Schnabel, SU Reichl, P Kranke, et al. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomised controlled trials. British Journal of Anaesthesia 2010; 105: 842-52
- Bhatnagar S, MishraS, Madhurima S, et al. Clonidine as an analgesic adjuvant to continuous paravertebral bupivacaine for post-thoracotomy pain. Anaesthesia and Intensive care 2006; 34: 586-91
- M Scarci, A Joshi, R Attia. In patients undergoing thoracic surgeryis paravertebral block as effective as epidural analgesia for pain management? Interactive Cardiothoracic and Vascular Surgery 2010; 10: 92-96
- MJ Eason and R Wyatt. Paravertebral block- a reappraisal. Anaesthesia 1979; 34: 634-42
- DJ Daly and PS Myles. Update on the role of paravertebral blocks for thoracic surgery: are they worth it? Current Opinion in Anesthesiology 2009; 22: 38-43
